June is Cataract Awareness Month
Cataracts are the result of the normally clear lens in your eye becoming cloudy. They can vary from extremely small areas of cloudiness to large opaque areas that cause a noticeable reduction in vision. Cataracts happen to almost everyone as they age, and are most often found in those over 60. If a child is born with a cataract, it is referred to as congenital.
Cataracts may develop slowly over many years or they may form rapidly in a matter of months. They develop without pain or redness. A full eye exam with an optometrist can determine if you have cataracts.
Symptoms of Cataracts
Is your vision blurry or foggy?
Do you have decreased night vision or see halos around lights?
Do colours appear dull or muted?
Do you feel as if there is a film covering your eye, but repeated blinking does not make it go away?
Does sunlight or other light seem overly bright or glaring?
Prevention
While no one presently knows how to prevent cataracts, you can slow their growth by wearing sunglasses that protect from UV rays and eat foods rich in antioxidants.
Treatment
In the early stages of a cataract, where vision is minimally affected, your optometrist can sometimes prescribe new lenses for your glasses to give you the sharpest vision possible. When the cataracts start to interfere with your daily activities and glasses cannot improve this vision, your optometrist will refer you to an ophthalmologist (eye surgeon) who may recommend the surgical removal of the cataracts.
Cataract surgery is a very safe and effective procedure to remove the cloudy crystalline lens from the eye and replace it with a clear implant. However, there are risks and limitations that should be discussed with an optometrist or ophthalmologist prior to undergoing the procedure.
During cataract surgery, the old cloudy lens is removed and an intraocular lens implant is inserted in your eye that serves as a new lens. Sometimes the lens implant can give you good enough distance vision that you may not need glasses. However, your near vision will still be blurred, so you will likely still require glasses to read. Your optometrist will prescribe new lenses for your glasses about four weeks after surgery to maximize your distance and near vision.
If you are experiencing the symptoms of cataracts, book an appointment with an optometrist right away.
What Does 20/20 Mean?
If you’ve been postponing regular visits to a doctor of optometry because they once told you that you had 20/20 vision, then you should keep reading.
“I have 20/20 vision” are words you may have uttered while bragging about having tip-top eyesight, however, it’s not that simple. In fact, it’s highly probable that many people don’t even know what those numbers means. 20/20 vision only represents the clarity of your vision when viewing objects 20 feet in the distance, CNIB explains:
Normal vision is known as “20/20”. This simply means that the eye being tested is able to see an object at 20 feet as well as any eye with very good vision. If you have 20/60 vision, this means you can see at 20 feet what a person with good vision can see at 60 feet. … if the change in vision is to 20/200 or worse, the person will still keep some vision but will be classified as “blind”.
Optometrists take multiple factors into consideration when determining the quality of your vision. A few of those factors include eye focusing, coordination, movement, teaming, as well as visual perceptual skills and color vision.
It should be noted that the quality of your eyesight and eye health are not mutually exclusive. Glaucoma, a progressive eye disease caused by increased pressure in the eye, demonstrates that you can have all the signs of good vision while unknowingly living with an eye disease that is one of the leading causes of blindness in Canada.
To stay in the know about the true state of your vision and eye health, make sure to book regular visits with your local doctor of optometry.
Glaucoma, The Silent Thief of Sight
Glaucoma is one of the leading causes of blindness in Canada. Glaucoma is a group of eye diseases which lead to progressive degeneration of the optic nerve. This in turn can lead to loss of nerve tissue that results in gradual irreversible vision loss and potential blindness if not detected and treated early.
The most common form of glaucoma is primary open angle glaucoma. This form is associated with elevated pressure caused by a backup of fluid in the eye.
What causes glaucoma?
The precise cause is unknown. Glaucoma is generally associated with increased fluid pressure in the eye, however, damage can also occur when eye pressure is normal; this is called normal pressure or normal tension glaucoma. Some theories point to an inadequate blood supply or poor perfusion.
Will I go blind from glaucoma?
If glaucoma is diagnosed at an early stage, treatment such as medication, eye drops and/or laser surgery can usually control or prevent further vision loss. If left untreated, some form of permanent vision loss is likely to occur.
How is glaucoma detected?
The most common type of glaucoma is primary open-angle glaucoma. It develops painlessly and gradually and there are no early warning signs. Pressure in the eye slowly rises and unfortunately, the cornea adapts without swelling. If the cornea were to swell, which is usually a signal that something is wrong, there would be symptoms. Since this is not the case, this disease often goes undetected. It is painless, and the patient often does not realize that he or she is slowly losing vision until the later stages of the disease. However, by the time the vision is impaired, the damage is irreversible.
In other cases, glaucoma may appear suddenly and present warning signs and symptoms such as nausea, eye pain, red eyes, blurred vision and haloes around lights. This is called acute angle-closure glaucoma.
A comprehensive eye examination is often the only way to detect glaucoma. Your doctor of optometry will perform a simple and painless procedure called tonometry during your routine eye exam, which measures the internal pressure of your eye. Your optometrist will also look into your eye to observe the health of the optic nerve and retina, and inspect the drainage angle He or she may also use specialized equipment to measure your field of vision additional imaging machines to examine the optic nerve and retinal layers.
Who Gets Glaucoma? – Risk Factors
Age - People over the age of 60 are at increased risk for the disease with the risk of developing glaucoma increasing slightly with each year.
Family history - Having a family history of glaucoma increases the risk of developing glaucoma.
Medical conditions - Some studies indicate that diabetes may increases the risk of developing glaucoma, as does variations in blood pressure (high and low) and heart disease.
Physical injuries to the eye—Severe trauma, such as being hit in the eye, can result in immediate increased eye pressure and future increases in pressure due to internal damage. Injury can also dislocate the lens, closing the drainage angle, and increasing pressure.
Other eye-related risk factors—Eye anatomy, namely corneal thickness and optic nerve appearance indicate risk for development of glaucoma. Conditions such as retinal detachment, eye tumors, and eye inflammations may also induce glaucoma. Some studies suggest that high amounts of nearsightedness may also be a risk factor for the development of glaucoma.
Corticosteroid use - Using corticosteroids for prolonged periods of time appears to put some people at risk of getting secondary glaucoma.
How is glaucoma treated?
Medications - A number of medications are available to treat glaucoma. Usually, these medications are intended to reduce elevated intraocular pressure. A single medication may be prescribed or a combination of medications. The type of medication may change if it is not providing enough pressure reduction or if side-effects are being experienced.
Surgery - All procedures attempt to reduce the pressure inside the eye. Surgery may help lower pressure when medication is not enough, however it cannot reverse vision loss.
Laser surgery - Laser trabeculoplasty helps to drain fluid out of the eye. A laser beam is used to stimulate the trabecular meshwork (an area of tissue in the eye located around the base of the cornea, near the ciliary body. It is responsible for draining the eye) to help it to work more efficiently at fluid drainage. The results may be somewhat temporary, and the procedure may need to be repeated.
Conventional surgery – If medication and laser surgery aren't effective in controlling eye pressure, a filtering procedure called a trabeculectomy may be required. Filtering microsurgery involves creating a drainage flap, allowing fluid to percolate into and later drain into the vascular system.
Drainage implants - Another type of surgery, called drainage valve implant surgery, may be appropriate for people with uncontrolled glaucoma, secondary glaucoma or for children with glaucoma. A small silicone tube is inserted in the eye to help drain aqueous fluid.
Treatment with daily eye drops and/or laser surgery is usually effective at maintaining your vision, but once vision is lost due to glaucoma, it cannot be restored. Patients with glaucoma must continue treatment for the rest of their lives. Since the disease can progress or change silently, compliance with treatment and eye examinations are essential. Treatment may need to be adjusted periodically.
Regular eye examinations with your optometrist are highly recommended to screen for and prevent glaucoma.
From an article on opto.ca
The Benefits of Regular Eye Exams
At first glance, many think a comprehensive eye exam is just a vision test, but, getting your eyes checked can have benefits that go well beyond the optometry chair.
Because of the eye’s small nerves and blood vessels, delicate structures, and close proximity to your brain, a comprehensive eye exam is one of the least invasive steps you can take to protect your overall health. Not only can your optometrist assess your eye health, they can identify symptoms of conditions elsewhere in the body, such as:
Brain Injuries and Neurological Conditions
The optic nerve in the eye is essentially an extension of the brain. Any neurological condition that affects nerve cells including Parkinson’s disease and multiple sclerosis can be detected with an eye exam.
High Blood Pressure
The fine blood vessels in the retina at the back of the eye can help identify risks of a stroke or heart attack before they occur.
Diabetes
As many as one million Canadians are living with undiagnosed diabetes. Optometrists sometimes see indicators of diabetes in the eyes before the disease is formally diagnosed because diabetes can damage the small blood vessels in your retina.
Cancer
Tests of peripheral vision and eye muscle function can often be the first line of detection of a brain tumor. A comprehensive eye exam can also identify unusual structures and growths within the eye. The eye and its surrounding tissues are one of the most common areas of the body where skin cancer is first diagnosed.
Regular comprehensive eye exams are an excellent way to monitor your overall health and catch certain issues early. Book your appointment today with Dr. Kwasnek (OD) at Grapevine Optical in Oliver by calling 778-439-3003.
From an article by the Canadian Association of Optometrists.
How to Protect Your Eyes in Winter
Before you wax your snowboard and sharpen your skates, you should ensure you’re taking the proper precautions to protect your eyes from tough winter weather.
Here are some eye safety tips you should consider this winter:
Feeling dry? Cold winter air holds less humidity, drying out our skin and eyes. If you’re experiencing excessively watery eyes, blurry vision and/or the desire to close your eyes, you may be experiencing dry eye. Try using a humidifier this time of year and ensure that the vents in your vehicle aren’t blowing directly at you.
Goggle up. Whether it is polarized lenses for snowboarding, or sunglasses to avoid debris and sunlight while snowshoeing, make sure to protect your peepers! Most people are unaware that excessive wind exposure can cause the white part of the eye to become irritated, which can lead to permanent yellow discolouration – also called pinguecula.
Sport your sunglasses. Despite the dropping temperature and increased cloud cover, it’s important to always protect your eyes against UVA and UVB rays. Your eyes are sensitive to these rays all year round, and we don’t often consider the reflections of the sun off the snow. Overexposure to UV rays has been linked to a multitude of problems, including cataracts, degeneration of the retina, and damage to the cornea. Be sure to select quality specs that have 100 per cent UVA/UVB stickers.
Come on in to Grapevine Optical to talk with our experts regarding products to protect your eyes, including sport sunglasses, prescription goggles, eye drops and more.
What Is Blue Light? Should I Be Worried About It?
These days 60% of people spend more than 6 hours a day looking at a digital device that emits blue light. But what is blue light? Should you be concerned about the blue light streaming into your eyes?
What Is Blue Light?
Blue light has very short, high-energy waves. In fact, they’re only slightly longer and less powerful than ultraviolet (UV) waves (which are too short for people to see with the naked eye). Health experts have warned against the harmful effects of UV rays, which can damage your skin and your eyes. High-energy blue light waves are nearly as powerful.
Blue light, like other colors of visible light, is all around you. The sun emits blue light. So do fluorescent and incandescent light bulbs. Human beings are exposed to more blue light than ever because of the widespread use of devices that rely on light-emitting diode (LED) technology. Computer and laptop screens, flat-screen televisions, cell phones, and tablets all use LED technologies with high amounts of blue light.
How Does Blue Light Affect Your Eyes?
Your eye is equipped with structures that protect it from some kinds of light. Your cornea and lens protect the light-sensitive retina at the back of your eye from damaging UV rays, for example. Those structures don’t keep out blue light. And you’re exposed to a lot of it — the natural blue light from the sun far exceeds the amount from any one device. Nevertheless, some ocular health experts have expressed concern about exposure to blue light from back-lit digital screens and devices because people spend so much time using them at such a close range.
Using digital devices up close or for long periods can lead to digital eye strain. Research has shown that when people use computers, laptops, and other digital devices, they tend to blink less often than normal. Fewer blinks can mean less moisture and more strain on your eyes. When your eyes are strained from staring at a blue-light-emitting screen, you might notice:
dry eyes
sore or irritated eyes
tired eyes
headaches
facial muscles fatigued by squinting
Exposure to blue light in the evening hours disrupts your sleep cycle, which can cause other problems such as an elevated risk of hormone-related cancers and metabolic changes.
What Can You Do?
Practice the 20/20/20 strategy. While you’re using a device that emits blue light, stop every 20 minutes to focus on objects that are around 20 feet away. Study those objects for 20 seconds before you return to your up-close viewing.
Keep your eyes moist. Eye drops, such as artificial tears, and room humidifiers are all good ways to keep your eyes from becoming too dry and irritated while you’re using blue-light-emitting devices.
Wear blue light blocking glasses. A blue lens blocking filter is designed to reduce blue light entering your eyes without any colour distortion. They are an affordable and effective strategy to reduce digital eye strain and improve your sleep.
At Grapevine Optical we can add blue light filters to almost any lense type and prescription. Give us a call or come in to find out more!
Staying Safe and Spooky
Cosmetic Contact Lenses - Be Safe, Not Sorry!
Cosmetic contact lenses are particularly popular at Halloween. Like contact lenses for visual correction, cosmetic contact lenses are classified as medical devices, and can pose a risk of harm due to improper fit, use, or care. Complications can be serious, including vision loss. See a licensed eye care professional, such as an optometrist, to properly fit your cosmetic contact lenses. Read the instructions that accompany any package of cosmetic contact lenses to help minimize the risks associated with these medical devices. If blurred vision, redness, discomfort, swelling or discharge occurs, stop using the lenses immediately and see your doctor of optometry.
Ensure Make-up Is Safe
Use products that are hypo-allergenic and make sure that any additives to the face paint are approved (check the recalls list at Health Canada if you are unsure). When applying make-up near or around the eye, stay away from the lid, or lash line—the area where you would normally apply eye liner. If you are applying make-up very close to the eye, use only products approved for use in that area such as an eye-liner or eye shadow. Do not use blush or lip-liner to create a "red" effect, as some ingredients may not be approved for use in the eye and bacteria from the mouth can be transmitted to the eye.
Keep Costumes Safe
Avoid sharp or pointy objects such as swords in costumes. If your child must carry a sword, makes sure it is secured to the outfit. If your child does get poked in the eye, thoroughly inspect it for any signs of redness, decreased vision or pain. Eye injuries may be more serious than they appear. If your child reports pain or blurred vision in the eye or if the eye is discolored or bloodshot, you should take your child to see a doctor of optometry as soon as possible. Ensure masks do not obstruct vision.
Be Seen After Dark
Use reflective tape and stickers on costumes and treat bags to increase visibility. Take a flashlight or wearable LED light so you can see and been seen.
Stay safe and have a fun Halloween!
Buying Glasses Online
If you have thought about purchasing your next pair of prescription eyeglasses online, there are a few things you need to know.
Ordering eyeglasses online may seem easy, but it is very different than ordering your average consumer item. It is important to know that your optometrist is trained in the proper fitting, measuring, manufacturing and dispensing of eyewear. When ordering online, the consumer is, in essence, taking on the role of a trained optical dispenser. This includes taking critical measurements and making critical decisions with respect to frame, lens and material selection. There is an inherent risk associated with making these determinations without the proper skills and education. Your prescription given to you by your doctor of optometry is only one piece of information that will determine how well you see with your new eyewear. During the normal process of selecting and getting properly fit for your new eyeglasses, your doctor of optometry is determining a number of things to make sure your new purchase is custom made to give you clear and comfortable vision, while making sure you look great, including:
Accurately measuring the distance between your pupils so that your new lenses will be properly located in the new frames relative to your eyes
Selecting the right size of frame for you
Selecting the right shape of frame for you
Determining what curvature of lens to use
Determining what type of lens material to use
Determining what coatings to use on your lenses that best suit your needs
Determining the height to place the optical center of the lens in your frames
Measuring how high to place the bifocal or progressive (if you wear a multifocal lens)
Properly adjusting the frame to your face
If all of the above are not chosen specifically for you, it’s not uncommon to have problems that begin immediately or develop after using your new eyeglasses for an extended period of time. Common complaints regarding improperly ordered or fit eyewear can include headaches, fatigue, an “eye pulling” sensation, nausea, and pain or pressure marks on your nose or around your ears.
Come into Grapevine Optical to have our experienced eyewear specialists help you select the perfect pair of glasses for you!
From an article by the Canadian Association of Optometrists.
Does my child need glasses?
There are a few signs that may indicate a child needs glasses. For example, squinting the eyes when trying to focus, tilting of the head, rubbing the eyes or covering one eye while reading or watching television may be signs of an uncorrected refractive error and the need for glasses. Children may also complain of blurry vision at a particular distance, or they may have trouble in school. If the two eyes are not working well together, a lazy eye can develop and may cause double vision. If caught early, this can be managed and treated with eyeglasses. It is a good idea to have children’s eyes checked as early as 6 months of age.
Book an appointment with Dr. Kwasnek ($0 with valid BC Health coverage!) to determine if there is any need for glasses or if there are any signs that glasses may be needed in the future. It is especially important for a child to be seen before starting school and yearly afterwards to ensure that they have optimal vision for learning.
What is Astigmatism?
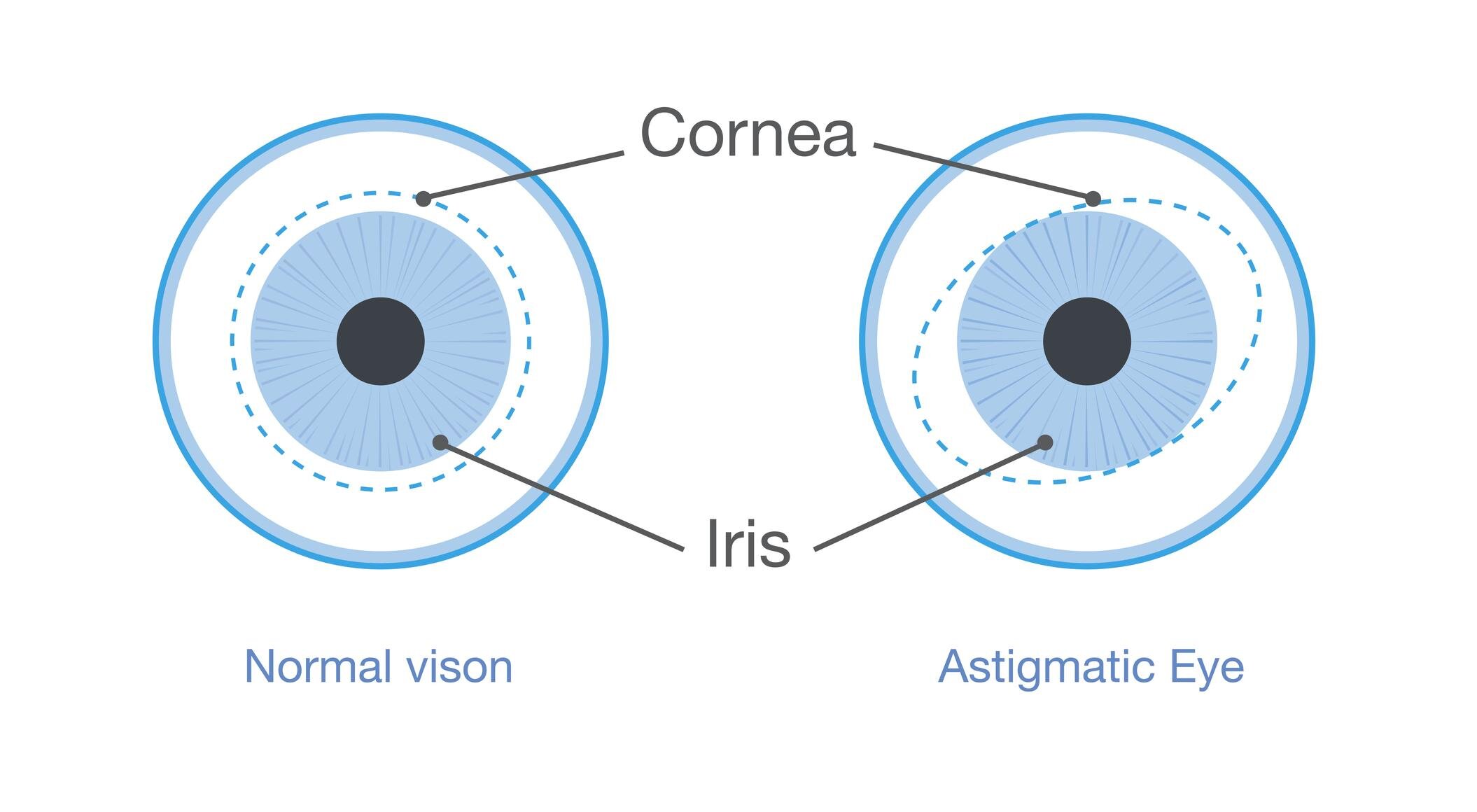
Example of vision with Astigmatism. It is a type of refractive error in which the eye does not focus light evenly on the retina. This results in distorted or blurred vision at all distances
Astigmatism is not a disease but a common vision condition that causes blurred vision. Most people have some degree of astigmatism. Small amounts of astigmatism do affect vision but may not require treatment. Larger amounts can cause distorted vision, eye discomfort and headaches.
This refractive error occurs when the front surface of the eye (cornea) or the lens inside the eye is slightly irregular or cylindrical in shape. An irregularly shaped cornea or lens prevents light from focusing properly on the retina, resulting in vision being blurred or distorted at all distances.
Astigmatism often occurs with other vision conditions like nearsightedness (myopia) and farsightedness (hyperopia). Collectively, these vision conditions are referred to as refractive errors because they affect how the eyes bend or "refract" light.
What causes astigmatism?
Astigmatism occurs when the front surface of the eye (the cornea) or the lens inside the eye is more oval or cylindrical than round. The cornea and lens are mostly responsible for properly focusing light entering your eyes. This allows you to see things clearly. Astigmatism is caused by small differences in the growth and alignment of the components of the eye. Genetics may play a role in the development of refractive error. Astigmatism may also result from such factors as pressure of the eyelids on the cornea.
Sometimes astigmatism develops following an eye injury or eye surgery. In rare cases there is also a condition called keratoconus that may occur. Keratoconus is a condition in which the cornea becomes progressively thinner and cone shaped. This causes a large amount of astigmatism resulting in poor vision that cannot be effectively corrected with glasses. In these cases, the clearest vision is achieved with contact lens wear. Corneal transplants or other corneal treatments may be considered, depending on the case
Astigmatism often occurs early in life, so it is important to schedule children for a comprehensive eye exam with an optometrist to avoid vision problems in school from uncorrected astigmatism.
How is astigmatism diagnosed?
Astigmatism is detected using the same instruments and tools used to detect farsightedness and nearsightedness. A doctor of optometry (optometrist) can determine the amount of astigmatism present by measuring how the eyes focus light. They can then determine the power of any optical lenses needed.
Astigmatism Correction Options
Almost all levels of astigmatism can be optically corrected. There are several corrective options available:
properly prescribed and fitted eyeglasses
contact lenses
laser and other refractive surgery
From an article by Canadian Association of Optometrists
Eye Openers
Did you know….?
Did you know that…?
the average blink takes 1/3 of a second.
Seeing is so important that it takes up more than 50% of the brain’s functionality.
Newborns don’t shed tears, though they do know how to cry.
You blink about 15-20 times in a minute.
The most active muscles in your body are in your eyes.
Your eyes can get sunburned.
Blue eyed people are more tolerant of alcohol and less tolerant of the sun
If the human eye were a digital camera it would have 576 megapixels.
We spend about 10% of our wake time with our eyes closed.
An ostrich’s eye is bigger than its brain.
Chameleons can move their eyes in two directions at once.
A single scallop can possess over a hundred eyes
Your eyes contain around 107 million light sensitive cells.
Dolphins can sleep with one eye open.
Birds, cats and dogs have three eyelids.
Yes, you can sneeze with your eyes open and no, your eyes won’t fall out.
Ommatophobia is the fear of eyes.
Humans can see more shades of green than any other colour.
The world’s most common eye colour is brown.
Dogs cannot distinguish between red and green.
The lifespan of the average eyelash is 5 months, the rest of your hair will last 2-4 years.
The eye has over 2 million moving parts.
Your eyes contain 7 million cones which help you see colour and detail and 100 million cells called rods which help you to see better in the dark.
From an article published by the Canadian Association of Optometrists.